Resilience in people with multiple sclerosis
Autor:innen:
Assoc. Prof. Mag. Priv.-Doz. Dr. Daniela Pinter1
Birgit Helmlinger, BSc, MSc1
Stefanie Hechenberger, MSc1
Manuel Leitner, BSc, MSc2
Dr. Sebastian Wurth2,3
Dr. Anna Damulina2
Dr. Rina Demjaha2,4
Assoc. Prof. Priv.-Doz. Dr. Michael Khalil2,4
Univ.-Prof. Priv.-Doz. Dr. Christian Enzinger2
1 Research Unit for Neuronal Plasticity and RepairMedical University of Graz
2 Department of NeurologyMedical University of Graz
3 Division of Neuroradiology & Interventional Radiology, Medical University of Graz
4 Neurology Biomarker Research Unit
Medical University of Graz
E-Mail: daniela.pinter@medunigraz.at
Psychological resilience describes “the process of managing and adapting to significant sources of stress, adversity, and challenging events”. It might play a key role in alleviating the physical and emotional distress associated with chronic illnesses such as multiple sclerosis (MS).
Keypoints
-
Our findings demonstrate that resilience significantly predicts key neuropsychological symptoms in MS over 1.8 years, accounting for up to 21% of variance in fatigue, anxiety and depression. This emphasizes the importance and potential to foster resilience in pwMS, through interventions like psychoeducation, cognitive-behavioral therapy, or online training programs.
-
Routine assessment of resilience could help to identify people most likely to benefit from psychological support, aiding them in managing the challenges of the disease.
Background
The American Psychological Association defines psychological resilience as “the process and outcome of successfully adapting to difficult or challenging life experiences, especially through mental, emotional, and behavioral flexibility and adjustment to external and internal demands”. Therefore, resilience can be understood as a set of protective factors and skills (such as coping strategies and social support) to overcome adversity.
Furthermore, the World Health Organization (WHO) has emphasized resilience as a key focus area, as evidence suggests it may help to mitigate the physical and emotional distress associated with chronic illness, including neurodegenerative diseases such as MS.1
MS is a neuroinflammatory disease of the central nervous system, leading to demyelination and neuronal damage, and is a major cause for non-traumatic disability among young adults aged 18–40 years.2 MS is profoundly heterogeneous regarding its clinical course, neuroradiological appearance, extent and distribution of lesions, and response to therapy. Due to this variability, people with MS often face significant uncertainties, which may contribute to a higher prevalence of depression and anxiety compared to the general population.
Cross-sectional studies showed that higher psychological resilience is linked to better physical and psychological outcomes in MS, including healthy aging,3 increased motor strength and gait,4 reduced fatigue,5 less severe depressive symptoms,6 and lower anxiety.7 Resilience is also thought to influence treatment efficacy.8
Despite these promising findings of higher resilience for physical, emotional, and mental dimensions, longitudinal studies of resilience in MS are scarce. Therefore, we aimed to explore the predictive power and potential longitudinal changes of resilience for key neuropsychological symptoms in people with MS.
Methods
We analysed longitudinal data from 122 people with MS (59% female; mean age=38 years; mean disease duration: 9.5 years, median expanded disability status scale [EDSS]=1) who underwent clinical and neuropsychological assessment at baseline and after a median follow-up time of 1.8 years.
We assessed resilience using the “Resilience Scale-13“. This questionnaire includes 13 items, each rated on a 7-point Likert scale (1=strongly disagree to 7=strongly agree), with total scores ranging from 13 to 91. Example items include: “I feel that I can handle many things at a time” or “My belief in myself gets me through hard times”.
We also evaluated key neuropsychological symptoms in MS. Fatigue (using the Fatigue Scale for Motor and Cognitive Function; FSMC), anxiety, depression (using the Hospital Anxiety and Depression Scale; HADS), and cognition (using the Brief International Cognitive Assessment for MS; BICAMS).
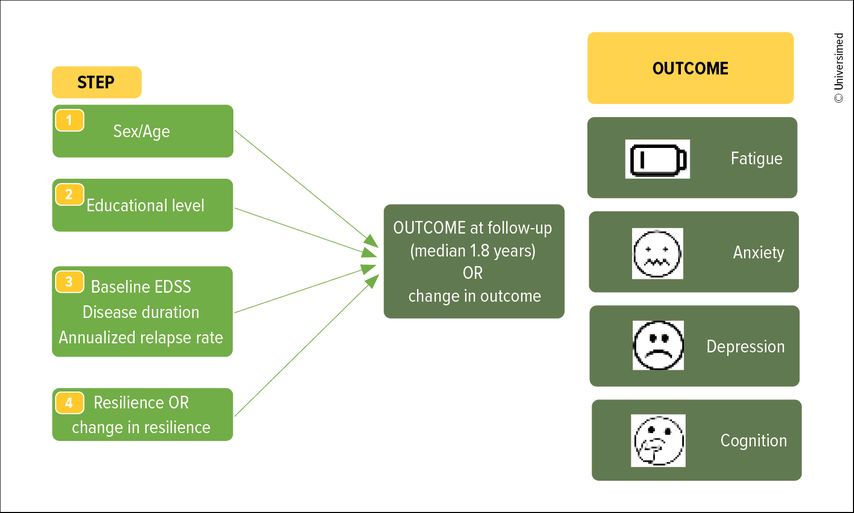
We conducted hierarchical linear regression models to predict fatigue, anxiety, depression levels, and cognition at follow-up. We used a step-wise approach, including potential demographic predictors (sex and age) in the first step, educational level in a second step, potential clinical predictors (baseline EDSS score, disease duration and annualized relapse rate) in the third step, before assessing the independent contribution of baseline resilience or “change in resilience” in the fourth step (Fig. 1). This approach enabled us to assess whether resilience contributes to prediction of outcomes independently and additionally from demographics and clinical factors.
Results
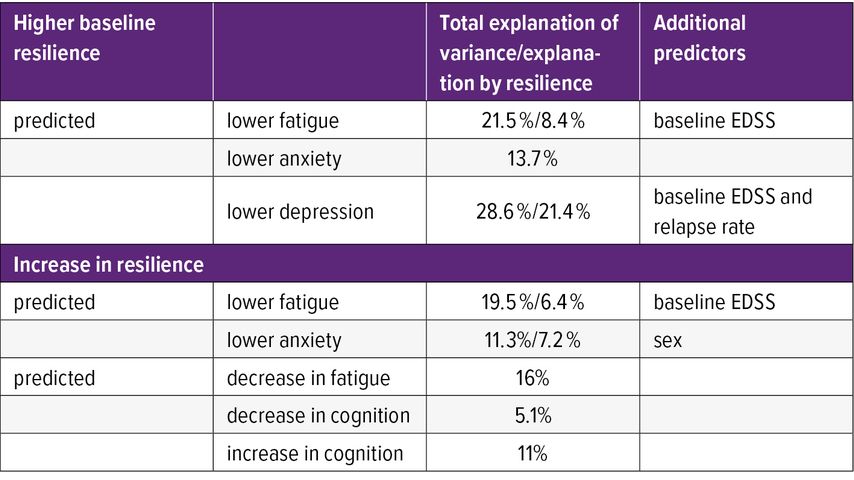
At baseline, about half of the participants (n=63; 51.6%) reported high resilience (>72 points). Higher baseline resilience contributed to prediction of lower fatigue, anxiety and depression at follow-up (Tab. 1). Severity of fatigue at follow-up was predicted by resilience (incremental adjusted explanation of variance [adjR2]=8.4%, with baseline EDSS [13.1%], total explained variance = 21.5%, p<.001). Resilience was the only significant predictor of anxiety (adjR2=13.7, p<.001). Resilience and EDSS predicted the level of depressive symptoms at follow-up (adjR2=21.4%, baseline EDSS and relapse rate (7.2%), total R2=28.6%, p<.001).
Resilience scores remained stable in 54 pwMS (44.3%) while 34 pwMS (27.9%) showed a meaningful decrease (>5 points) within the follow-up period of 1.8 years.
Changes in resilience contributed to the prediction of fatigue (adjR2=6.4%), baseline EDSS (13.1%, total R2=19.5%, p=.002), and anxiety at follow-up (adjR2=7.2%, sex [4.1%], total R2=11.3%, p<.001). Decrease in resilience was associated with higher fatigue and anxiety at follow-up. Furthermore, decrease in resilience contributed to increase in fatigue (adjR2=16%, p<.001) and depression (adjR2=5.1%, p=.005) and cognitive decline (adjR2=11%, p<.001) over time.
Conclusion
Our findings demonstrate that resilience significantly predicts key neuropsychological symptoms in MS, emphasizing the importance and potential to foster resilience in pwMS. Moreover, as changes in resilience across 1.8 years were linked to worsening of fatigue, depression and cognition, ongoing psychological support aimed at strengthening resilience – by enhancing coping skills and social support – may help to mitigate these effects.
The underlying mechanisms of the positive effect of high resilience on MS are not fully understood. One assumption is that resilience might facilitate adaptation to stressful events through various mechanisms, including a more effective neuroendocrine regulation abating inflammatory MS-related processes.9 Other groups suggest that the most important modifier of disability appears to be a healthy and active lifestyle, which is more common in persons with high resilience.10 Both mechanisms likely interact to offer protective effects.
Most importantly, resilience is malleable, and should be strengthened preventively11 to help mitigate the physical and emotional distress associated with MS.
Literatur:
1 Gallo A, Bisecco A: Psychological resilience explains functional variability across people with multiple sclerosis – commentary. Mult Scler 2021; 27(4): 506-8 2 Jakimovski D et al.: Multiple sclerosis. Lancet 2024; 403(10422): 183-202 3 Ploughman M et al.: The impact of resilience on healthy aging with multiple sclerosis. Qual Life Res 2020; 29(10): 2769-79 4 Klineova S et al.: Psychological resilience is linked to motor strength and gait endurance in early multiple sclerosis. Mult Scler 2020; 26(9): 1111-20 5 Ovaska-Stafford N et al.: Literature review: psychological resilience factors in people with neurodegenerative diseases. Arch Clin Neuropsychol 2021; 36(2): 283-306 6 Silverman AM et al.: Resilience predicts functional outcomes in people aging with disability: a longitudinal investigation. Arch Phys Med Rehabil 2015; 96(7): 1262-8 7 Battalio SL et al.: Resilience and function in adults with physical disabilities: an observational study. Arch Phys Med Rehabil 2017; 96(6): 1158-64 8 Zackowski K et al.: Prioritizing progressive MS rehabilitation research: a call from the International Progressive MS Alliance. Mult Scler 2021; 27(7): 989-1001 9 Leavitt MV, Kever A: Psychological resilience explains functional variability across people with multiple sclerosis - Yes. Mult Scler 2021; 27(4): 503-4 10 Ploughman M: Psychological resilience explains functional variability across people with multiple sclerosis - No. Mult Scler 2021; 27(4): 504-6 11 Joyce S et al.: Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018; 8(6): e017858
Das könnte Sie auch interessieren:
Blutbiomarker-Diagnostik in der klinischen Praxis: Anwendungsempfehlungen
Blutbasierte Biomarker (BBM) eröffnen neue Möglichkeiten für die frühzeitige Diagnostik der Alzheimererkrankung. Sie könnten die Identifikation von Patient:innen mit kognitiven ...
Optische Kohärenztomografie bei Multipler Sklerose – wie viel ist genetisch?
Mit der optischen Kohärenztomographie kann durch die Messung retinaler Schichtatrophie die neuroaxonale Schädigung bei Multipler Sklerose erfasst werden. Eine neue Studie gibt Einblick ...
APOE und Anti-Amyloid-Therapien: Genetik im klinischen Alltag
Mit der Zulassung der ersten krankheitsmodifizierenden Therapien hat ein Paradigmenwechsel in der Behandlung der Alzheimerkrankheit begonnen. Anti-Amyloid-Antikörper können den ...